Understanding the Fine Print Can Protect Your Medicare Benefits
When you’re in the hospital, everything may feel like an emergency—but there’s one critical detail that’s often overlooked: are you officially admitted or simply under observation? For patients on Medicare, this difference can affect your coverage, rehab options, and out-of-pocket costs in a big way.
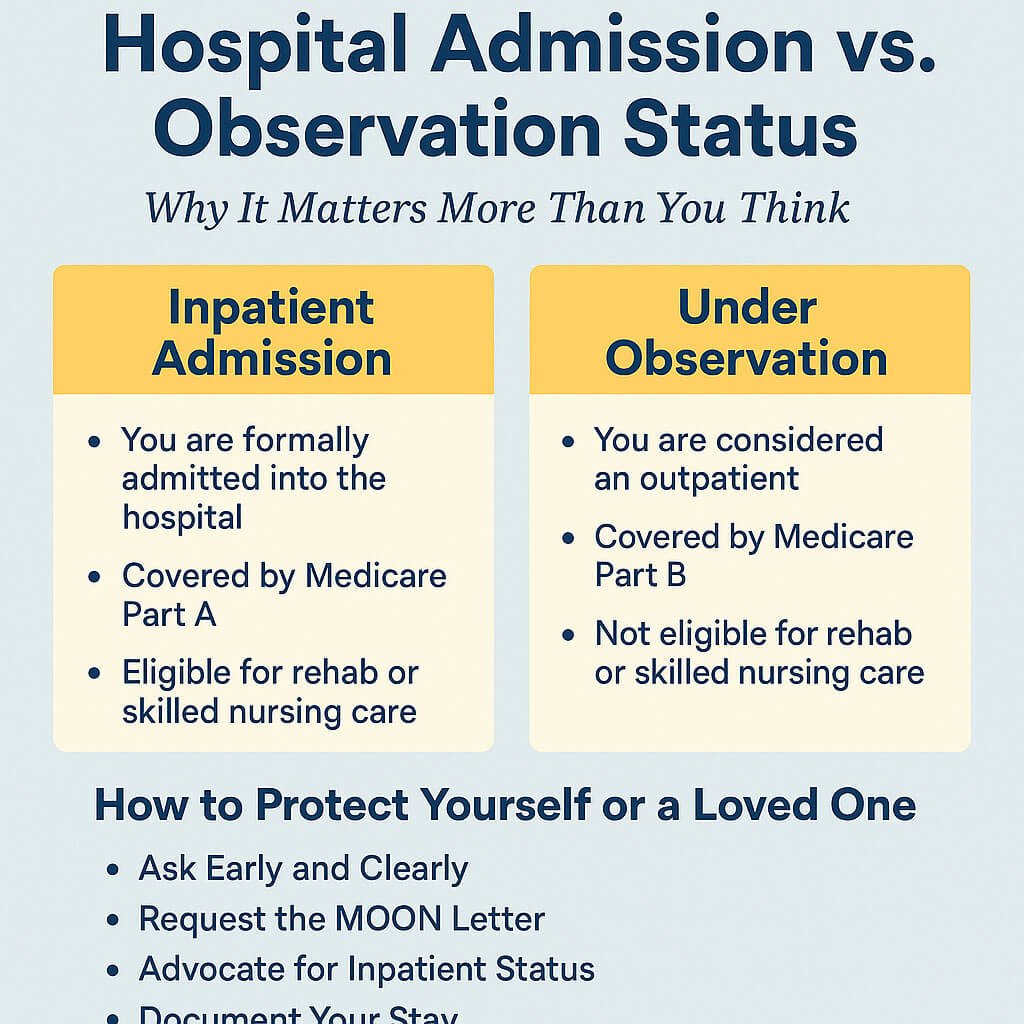
What's the Difference Between Hospital Admission and Observation?
- Inpatient Admission: You are formally admitted into the hospital, and your care is covered under Medicare Part A. After a 3-day inpatient stay, you’re eligible for Medicare-covered skilled nursing or rehab care.
- Observation Status: You’re technically classified as an outpatient, even if you stay overnight or longer. This is billed under Medicare Part B, and these days do not count toward qualifying for rehab or a skilled nursing facility.
Why Observation Status Can Hurt You
Many seniors are shocked to learn that time spent in the hospital “under observation” doesn’t meet Medicare’s 3-day inpatient rule. This means:
- No coverage for skilled nursing rehab afterward
- Higher out-of-pocket costs for tests, meds, and hospital care
- Surprise medical bills even after a multi-day hospital stay
According to Medicare.gov, observation status is one of the top reasons patients are denied coverage for necessary follow-up care.
How to Protect Yourself
Here are 5 ways to ensure you’re covered:
- Ask Early and Clearly: Ask, “Am I admitted as an inpatient, or under observation?” Don’t assume. Even if you’re in a hospital bed overnight, you may not be “admitted.”
- Request the MOON Letter: Hospitals are required to give you a Medicare Outpatient Observation Notice (MOON) if you’re under observation for more than 24 hours.
- Advocate for Inpatient Status: If your condition warrants it, your doctor may be able to change your status from observation to inpatient. This can make you eligible for rehab care after discharge.
- Document Your Stay: Keep notes on dates, times, who you spoke to, and any paperwork. This helps in case of billing disputes or appeals.
- Use a Trusted Advocate: Contact a NAOSA-certified professional or hospital case manager to help you navigate the system.
Final Tip: Know Before You Go
You or a loved one might not be thinking about Medicare technicalities during a health crisis—but understanding hospital status can mean the difference between thousands in coverage or out-of-pocket bills. Be proactive. Ask questions. Get it in writing.
Need help? Visit NAOSA.org for consumer alerts, advocacy tips, and a nationwide network of ethical professionals who protect seniors and their families.
Related Links:
- Skilled Nursing Facility Coverage – Medicare.gov
- MOON Notice Information – CMS.gov
- Find a NAOSA Professional – National Association of Senior Advocates


